Spinal vascular malformations are a group of blood vessel disorders any of which can lead to spinal cord dysfunction or damage. There are 4 subtypes of spinal vascular malformations and each one has unique causes and and different treatments.
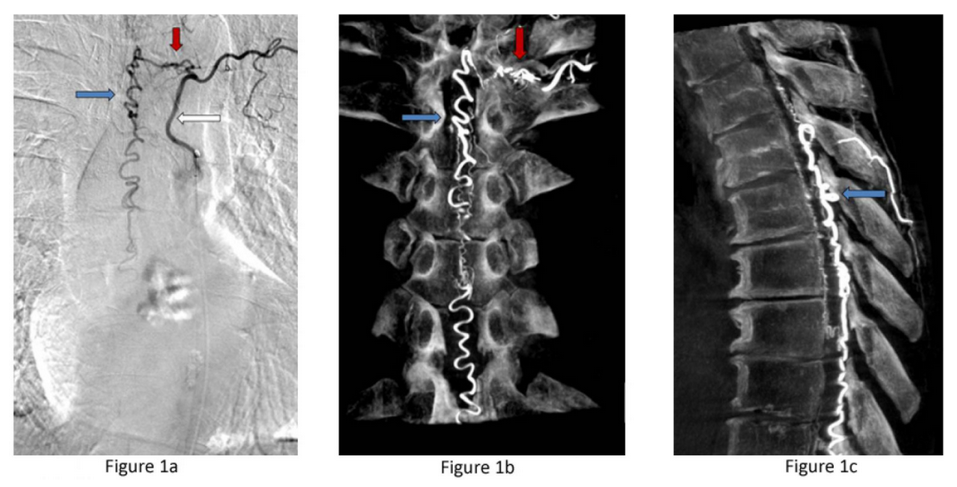
Figure 1a: Type I dural AV fistula – spinal angiogram of a left sided spinal artery (white arrow) showing an abnormal connection (red arrow) with a spinal vein that has become abnormally enlarged (blue arrow). Figure 1b: Similar view of the same fistula using a 3D flat panel CTA reconstruction showing greater detail of the abnormal artery-venous connection within the nerve root dural sleeve (red arrow) and enlarged vein within the spinal canal (blue arrow). Figure 1c: Side or sagittal view of the same fistula showing the enlarged vein (blue arrow) along the back wall of the spinal canal behind the spinal cord.
Spinal Dural Arteriovenous Fistulas (Type I): These lesions account for the 70% of spinal malformations and are the result of an abnormal connection between a dural artery and a vein within the spinal canal dura. The abnormal connection between the high pressure system of arteries and the low pressure network of veins creates high pressure in the vessels draining the spinal cord. The elevated pressure prevents blood leaving the spinal cord and damages the cord over time. Spinal dural fistulas occur spontaneously in adults and are neither inherited nor congenital. These wounds do not break or ooze blood, making them excellent candidates for surgical treatment.
Spinal Arteriovenous Malformations (Type II): Type II malformations, also known as glomus AVMs, account for 20% of spinal vascular malformations. Similar to brain AVMs, they are abnormal tangles of arteries and veins within the spinal cord itself. The AVM can bleed in the spinal cord and spinal fluid and also sudden weakness in the lower body.
Juvenile Arteriovenous Malformations (Type III): These are vascular abnormalities that include an arteriovenous malformation in the spinal bone, dura matter, and spinal cord. Because of their propensity to be big and high flow they are difficult to treat. These abnormalities are thought to develop in early fetal development.
Pial Spinal Arteriovenous Fistulas (Type IV): Pial AVFs are a rare malformation in which an artery and vein on the spinal cord’s surface connect. Due to high pressure from the abnormal connection to the artery, the vein grows larger over time and begins to compress the spinal cord.
The symptoms of spinal vascular malformations depend on the type of problem. Spinal dural fistulas (Type I) are especially crucial to detect since if left untreated, patients will gradually lose the use of their legs and become incontinent, but with prompt treatment, the consequences may be reversed.
Symptoms can be classified into two categories: a) progressive spinal cord impairment, and b) acute weakness caused by vessel bleeding.
Progressive Spinal Cord Dysfunction (Progressive Myelopathy) – Types I, IV and occasionally types II, III.
Over months to years, strength and sensation in the legs progressively declines and later, urinary incontinence occurs. It is difficult to walk long distances due to loss of sensation and weakness in the legs.
Sudden Weakness or Bleeding into the Spinal Fluid – Type II
Spinal AVMs can cause sudden weakness in the legs or arms and legs at the same time. A bursting of the unusual vessels into the spinal fluid can produce sudden, severe back discomfort described as a “stab in the back”. The pain often occurs at the same time as limb paralysis. Additionally, bleeding into the spinal fluid lead to one or more of the following symptoms:
- Nausea
- Vomiting
- Headache
- Neck stiffness
Physicians initially identify a spinal vascular malformation by looking at the patient’s symptoms. The physician may request the following tests based on the symptoms:
Spinal MRI: The sequence of this test is generally the first one used when a spinal vascular malformation is suspected. Spinal MRIs can reveal abnormal vessels, abnormalities in the spinal cord, and provide important information about the existence and position of the vascular abnormality.
Spinal Angiogram: The gold standard for detecting a spinal vascular malformation, determining the sort (Types I-IV) and demonstrating its precise position in the spine canal.
Spinal MRA or CTA: The following tests can be carried out at specialized clinics and may show the presence of vascular abnormalities. They do, however, provide less information than a spinal angiogram.
Depending on the type of spinal vascular malformation, the best management and treatment approach must be carefully determined to the individual patient by a specialized cerebrovascular neurosurgeon. Surgery or embolization is used in most cases.
Observation: Some spinal vascular malformations are in critical areas of the spinal cord, are not high risk and it is preferable to observe them.
Surgery: The majority of spinal vascular malformations (70%) are type I spinal dural fistulas which can be repaired surgically with a low risk to the patient (Type I lesions).
Endovascular Embolization: Depending on the lesion, there are cases where endovascular embolization is the best option.
Please see the treatments area for additional information on spinal vascular malformations procedures.
