Endovascular surgery is a minimally invasive treatment that has been used to treat many different neurovascular conditions such as aneurysms, vascular malformations, and other arterial conditions. It involves inserting a catheter into the artery and then using it to perform an angioplasty or stent placement. Endovascular Surgery offers many benefits over traditional forms of surgery such as faster healing times and smaller incisions.
Since its conception, endovascular treatment has rapidly taken over as the major treatment for most intracranial aneurysms including:
Endovascular coiling is the process by which an aneurysm is blocked with coils to stop blood flow. This is a minimally invasive procedure, meaning that instead of cutting into the skull to treat aneurysms in the brain, it’s done by inserting catheters up through arteries until it reaches the damaged area where platinum coils are released to coagulate (embolization) the aneurysm and prevent blood from entering it.
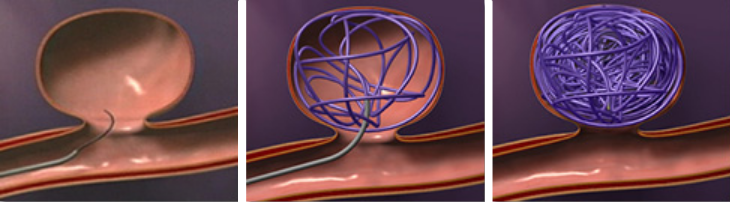
Figure 1. Endovascular coiling
Stent-assisted coiling is when coils are inserted alongside a stent to compress the aneurysm and seal it off from blood flow. The stent is placed across the base of the aneurysm to act as a scaffold to keep the coils in place.
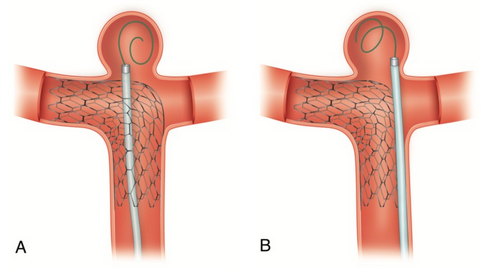
Figure 2. Stent-assisted coiling. (A) Coil-through struts technique. B) Jailing technique.
In the flow diversion procedure, a metal stent made with small holes is inserted across the base of an aneurysm. The stent diverts blood flow away from the aneurysm and encourages it to remain in its normal flow. Over several months, blood within the aneurysm clots due to sluggish flow, and the ruptured tissue heals, but the healthy artery remains open. This technique is often used for very large or difficult-to-treat aneurysms.
Rather than placing a device inside the aneurysm sac, such as with coiling, flow diversion is achieved by diverting blood flow away from the aneurysms themselves.
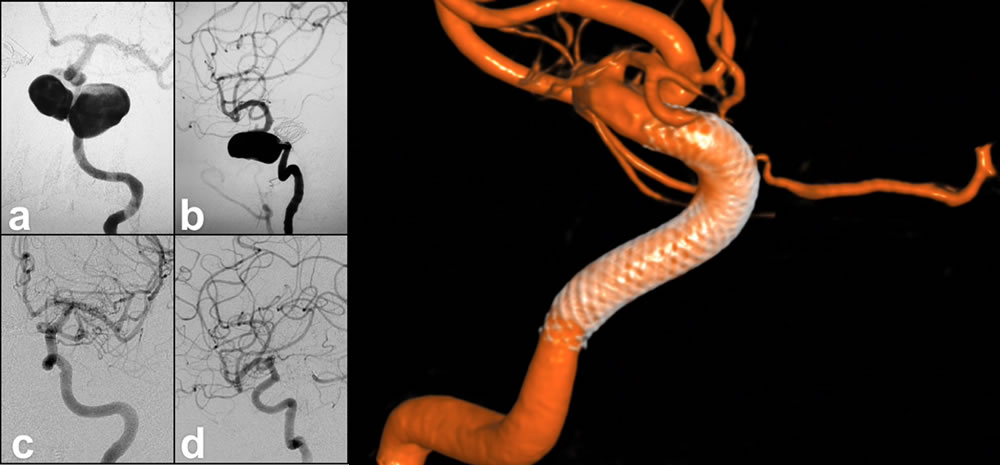
Figure 3. Giant, tri-lobed left ICA cavernous segment aneurysm pre-treatment (a) AP and (b) lateral angiographic views. Six months post-treatment with pipeline flow diverting stent shows complete obliteration of the aneurysm on (c) AP and (d) lateral views. (e) shows the pipeline stent in the vessel after the aneurysm has occluded.
Embolization is often used before neurosurgery to restrict blood flow through the AVM. This procedure consists of inserting very small tubes into the arteries of the brain and injecting a special glue-like liquid that will block the blood vessels in the AVM.
The procedure is performed while the patient is awake but sedated. A balloon catheter, guided by an X-ray, is placed in a blood vessel to reach the area of blockage or narrowing. At the area of blockage, the balloon tip opens and widens the artery. Then a special filter (called the embolic protection device) is put in to stop blood from clotting which collects any debris that may break off of the blockage. Finally, a stent is inserted into the artery, and it opens to be of a size that conforms to the size of the vessel.
Stents act as scaffolding and keep the artery open so blood flow is not obstructed. After several weeks, the tissue will grow around and fix to the stent.
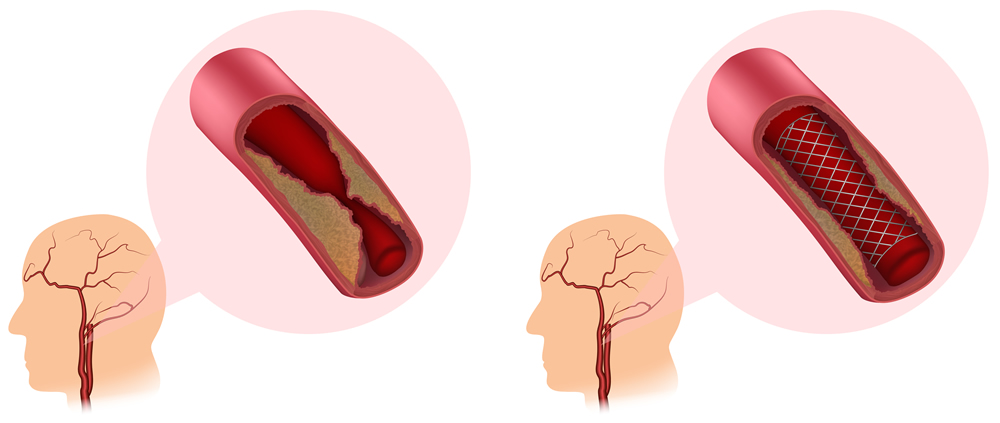
Figure 4. Carotid Artery Stenting
After ischemic stroke, endovascular therapy has been found to improve outcomes and reduce long-term disability. These operations must be done as soon as feasible:
Tissue plasminogen activator (tPA) delivered directly to the brain: To deliver tPA directly to the site of a stroke, an interventionalist uses a long, thin tube (catheter) to penetrate your groin and thread it into your brain. This therapy is somewhat longer than injected tPA in terms of time window, but it’s still pretty tight.
Mechanical Thrombectomy (mechanical blood clot removal): Patients are candidates when a major brain blood vessel is obstructed and the delay from the start of symptoms has been less than six hours, plus special brain scans reveal that no significant damage to the brain has occurred.
A neurointerventionalist uses a thin tube called a catheter to insert the probe. They place a long catheter, or thin tube, into the femoral artery in the leg and guide it up the vessel into the brain’s blood vessels with x-ray assistance. A catheter with a tiny diameter is used to inject dye through the tube and take x-ray pictures of blood vessels for an angiogram (x-ray picture of blood vessels).A grasping device is inserted into the clot via the catheter and used to physically remove the blockage from the brain, restoring blood flow to the brain. The brain can be kept from permanent harm if the vessel is opened in time. Even up to 24 hours after symptoms begin, stent retriever stroke operations are safe and highly effective in selected individuals.
Typically enough to cure most DAVFs. The doctor inserts a catheter through the blood vessels in the leg or arm, navigates the tubes under x-ray guidance up into the brain’s arteries that lead to the DAVF and injects liquid embolic chemicals such as NBCA, glue or Onyx into these arteries during this procedure. This injection seals off the artery and decreases blood flow through the DAVF or cures it.
Endovascular embolization is a minimally invasive radiological therapy that is used to reduce the chance of bleeding and other adverse effects associated with spinal AVMs.
In endovascular embolization, a catheter is inserted into a person’s artery in the leg and navigated to an AVM-feeding artery in the spinal cord. Small particles of a glue-like substance are injected to block the blood vessel and restrict blood flow into the AVM. The AVM isn’t permanently destroyed.
