Arteriovenous fistulas are connections between two vessels that are abnormal. Dural arteriovenous fistulas, or DAVFs for short, occur when perforating veins in the dura mater of the brain’s meninges connect an artery and a vein.
Arteries transport blood from the heart to the tissues, while veins carry blood from the tissues back to the heart. There is a direct link between one or more arteries and veins, or sinuses, in a DAVF, which leads to a slew of issues. Unlike arteriovenous malformations (AVMs), which are found within the brain or spinal cord, dural AVFs are located in the coverings of the brain or spinal cord called the dura mater.
The most dangerous effect of DAVFs is that they move high-pressure arterial blood into veins or venous sinuses, leading to an increase in the pressure of the vein system around the brain or spinal cord.
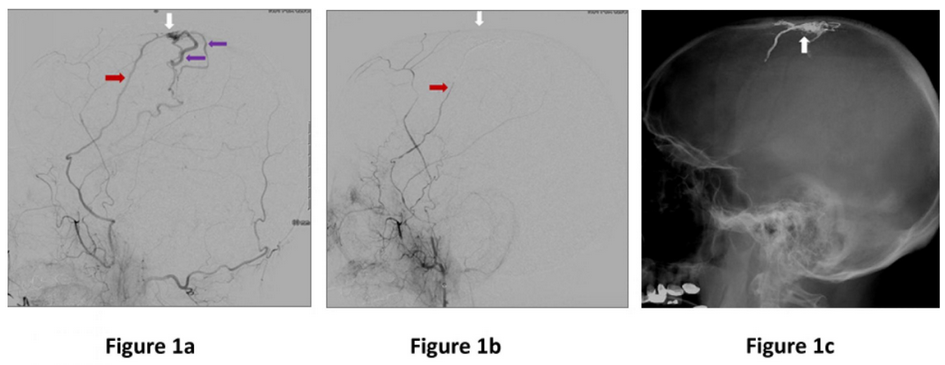
Figure 1a: Lateral (side) view of a dural artery (red arrow) abnormally connecting to a large vein on the surface on the brain (white arrow), and high pressure arterial flow is immediately filling brain veins (purple arrows). Figure 1b. Immediately after embolization where glue was injected through the artery (red arrow) into the abnormal connection (white arrow) showing no more abnormal filling of the veins. Figure 1c. Lateral (side) view skull x-ray showing the glue material filling the area abnormal connection of the fistula (white arrow).
Symptoms vary depending on the location of the fistula in the head but can include:
- Headache
- Pulsatile Tinnitus: A whooshing sound is often reported by patients with DAVFs near the ear, and it’s sometimes referred to as a high-pitched ringing noise often corresponding with the heartbeat.
- Eye symptoms: When the abnormal vessel-vein connection is near the eye, some patients experience pain in the back of their eyes, redness, puffiness, vision, loss and even double vision.
- Brain hemorrhage: Blood vessels in the brain that are abnormally large or narrow may cause bleeding into the brain. Those at risk include individuals with a DAVF that allows abnormal, high-pressure artery blood flow to enter veins of the brain directly. This is called cortical venous drainage (CVD) and is a hazardous condition.
- Sudden-onset headache, nausea, vomiting, loss of consciousness, weakness, numbness, and difficulty with speech are all signs of a brain hemorrhage.
- Seizures: Seizures can also occur in patients with CVD.
- Cognitive decline: Patients with long-standing, untreated DAVFs may experience cognitive deterioration, which is similar to dementia.
If a fistula is suspected, it’s critical to get appropriate testing and consult with a specialist as soon after the problem is confirmed. Based on the patient’s symptoms, the doctor may order one or more of these tests. Before coming to a decision about treatment, all of these procedures are frequently required:
Computed Tomography (CT) scans
Magnetic resonance imaging (MRI)
Cerebral angiogram: An angiogram, also known as an arteriogram, is a specific examination in which a neuroradiologist injects dye into the brain’s blood vessels and obtains pictures of them. The angiogram is currently the best test for detecting the DAVF and its relationship to the surrounding arteries and veins.
Treatment decisions will be made based on the AVF’s location, presence or absence of CVD, severity and type of symptoms, and the risk involved in treatment. Treatment options for brain AVFs include:
Observation: If a patient has an AVF without CVD and minor symptoms, observation is frequently advised.
Endovascular Embolization: The surgeon advances a small catheter into the abnormal blood vessel connection, then injects glue or other material into it to block the connection and cure the fistula. This is the most common approach to treat DAVF and can be curative.
Surgery: When embolization is not feasible or not the most effective option, microsurgery and direct ligation/resection of the AVF may be performed.
Radiosurgery: Radiotherapy, a treatment that uses precisely concentrating radiation beams on the AVF in order to shrink it over time, can be used when embolization and surgery fail.
See the treatments area for more information on dural arteriovenous fistulas therapies.
