Chronic subdural hematoma (cSDH) is an abnormal collection of blood products in the fluid space between the surface of the brain and the inner lining of the skull, called the “dura matter.” These types of blood product collections occur more frequently in older age groups due to the increased space between the brain surface and the dura matter. Chronic subdural hematoma collections are thought to begin as small bleeds after a minor trauma event such as bumping of the head, but the collections can slowly grow over time, particularly in patients who use blood thinners or have other medical reasons for easy bleeding. If the blood products become large enough, they result in pressure on the brain and result in symptoms (see Figure 1)
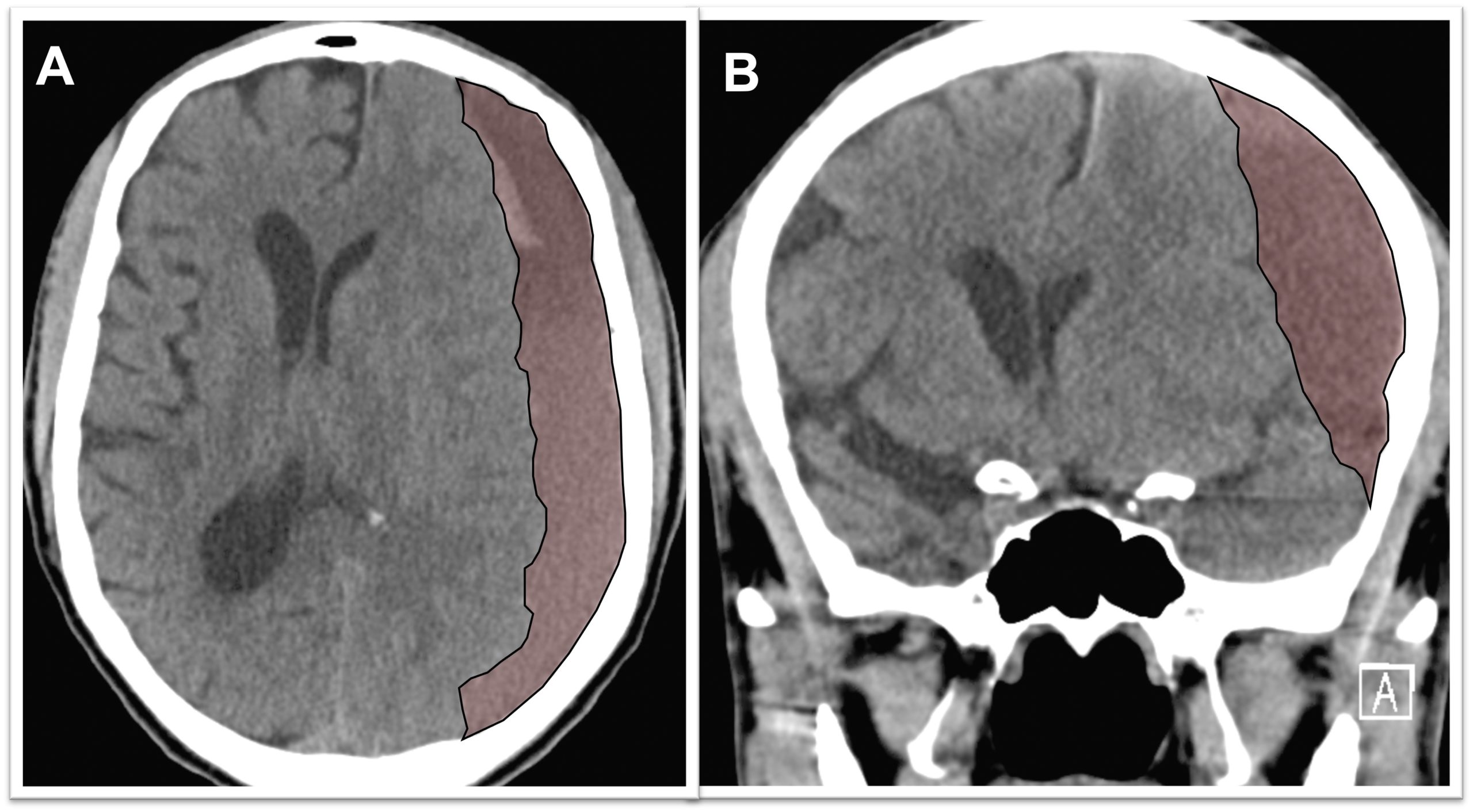
Figure 1. A)Axial view of a brain CT scan demonstrating a chronic subdural hematoma collection below the skull (the skull is bright white) shifting the brain (brain surface is marked with the yellow line) to the other side. B) Coronal view of the same patient demonstrating the chronic subdural hematoma occupying the subdural space and shifting the brain to the other side (brain surface marked with yellow line).
Symptoms from chronic subdural hematomas are often mild such as headaches but may slowly increase with time to include behavioral changes such as confusion or atypical behavior. Over time, these lesions can enlarge increasingly press on the brain leading to weakness on one side of the body, inability to walk, seizures and even coma.
After an injury in subdural space, the body attempts to remove the blood collection by forming a thin layer around it called subdural membranes. The membranes contain tiny newly formed blood vessels which allow the body’s immune system to remove the blood that has leaked into the subdural space. However, these small vessels in the membrane are also leaky, and in some patients, the membranes bleed more into the subdural space than they absorb. The net effect of this process in some patients is growth of hematoma over weeks to months until it becomes large enough to cause symptoms.
Certain factors may increase the risk of having a chronic subdural hematoma, including:
Mild Head Injury. Chronic subdural hematomas most commonly develop in the setting of a recent fall or minor head injury in an older patient or at-risk patient. The head jarring is believed to initiate factors leading to a chronic subdural hemorrhage that can grow with time.
Advanced Age. The older age groups are more at risk of developing chronic subdural hematoma due to brain volume reduction that is natural with ageing.
Blood Thinner Medications. Blood thinner medications increase the risk of bleeding in the space above the brain and below the dura (subdural space). Once a chronic subdural hematoma is detected, blood thinners are stopped.
Medical conditions. Certain medical conditions such as liver failure or renal failure can lead to poor clotting and increase the risk of bleeding.
Tools and techniques to diagnose chronic subdural hematomas.
CT Scan Brain – the most commonly and most useful diagnostic test for chronic subdural hematoma
MRI Brain – can see brain structures in more detail but is less useful in determining the age of the blood in chronic subdural hematoma.
Classically, treatment of chronic subdural hematomas was either with observation or surgical drainage of the blood products. These are the best management option for many patients. However, there is an alternative chronic subdural hematoma treatment option called Middle Meningeal Artery Embolization which has demonstrated good results resolving many chronic subdural hematomas without open surgery in select patients.
Middle Meningeal Artery Embolization – This procedure is performed in an endovascular intervention suite with the patient under sedation. The endovascular surgeon uses minimally invasive technique to enter the blood vessels in the arm or leg, advances small tubes through the arteries under x-ray guidance and navigates them to the middle meningeal artery on the side of the chronic subdural hematoma. The middle meningeal artery is located on the underside of the skull in the dura matter but also provides blood supply to the abnormal membranes that surround the hematoma and contribute to hematoma growth (see Figure 2). Under fluoroscopic guidance (low dose continuous x-rays), the surgeon delivers a specially made glue or small particles through the small tube and permanently blocks the middle meningeal artery. After the procedure, the tubes are removed and the small puncture site in the arm or leg artery is closed. In the weeks following the procedure, there is reduced bleeding from the subdural hematoma membranes and the hematoma collection slowly shrinks in size and often goes away completely over the course of several months (see Figure 3).
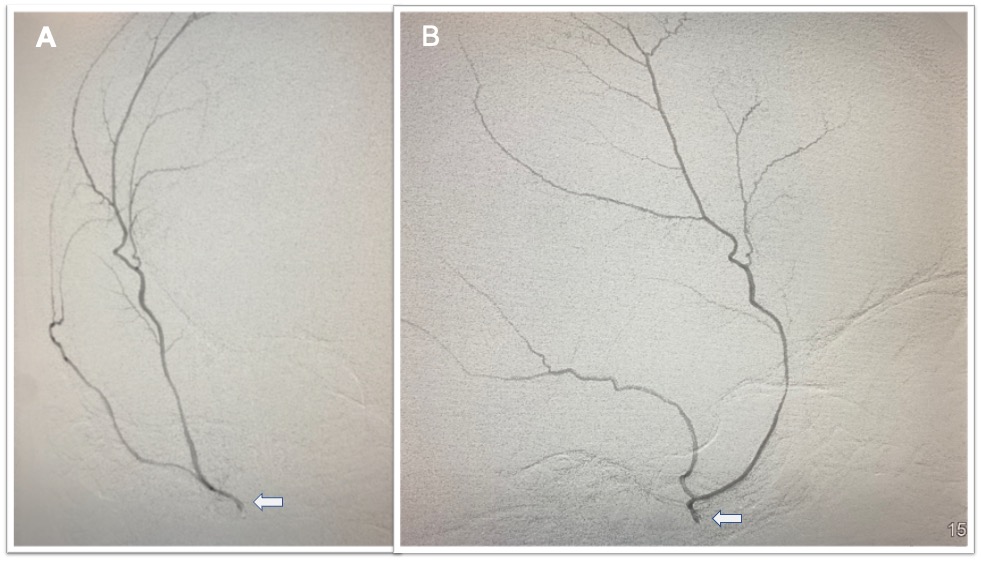
Figure 2. A) Anterior to posterior (front to back) view of the right side of the head with a microcatheter (tiny tube) in the right Middle Meningeal Artery (arrow) injecting contrast dye into the vessel which branches along the underside of the skull. B) The lateral view of the same microcatheter (arrow) injecting contrast dye filling the right Middle Meningeal Artery. This vessel was occluded to treat a chronic subdural hematoma.
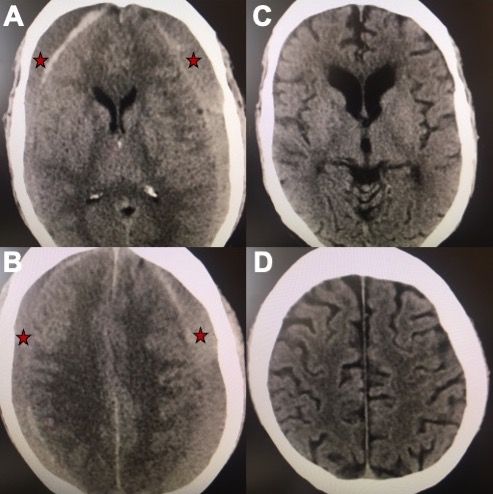
Figure 3. A, B) Axial views of a brain CT scan demonstrating chronic subdural hematomas on both sides of the brain compressing it inwards (red stars mark the hematoma). C, D) Axial views of a CT brain of the same chronic subdural hematoma 3 months after Middle Meningeal Artery Embolization demonstrating resolution of the chronic subdural collection on both sides.
Burrhole Drainage – This is the most common surgical procedure for treatment of chronic subdural hematomas and is performed in the operating room with the patient under general anesthesia. The procedure involves opening two holes, each about the size of a quarter, in the skull and draining the hematoma out. A drain is often left in the hematoma space for several days after surgery to maximize the drainage.
Craniotomy – This procedure is performed in the operating room by opening a larger area of the skull and directly removing the chronic subdural hematoma with surgical instruments and drainage. A drain is often left in the hematoma space for several days after surgery to maximize the drainage.
Middle meningeal embolization procedures for chronic subdural hematoma treatment are performed at Ronal Reagan UCLA Medical Center. Since the procedures are performed using minimally invasive technique, they can often be performed under sedation, rather than general anesthesia, and patients experience reduced discomfort and a shortened hospital stay compared to traditional surgery. After treatment, patients are monitored overnight in the hospital and may be discharged as early as the following day. At UCLA Health neurosciences, we employ highly specialized multidisciplinary health care teams, and in addition to innovative cutting-edge care, we provide support services for patients and their families to help navigate their time in our clinics and hospitals.
To schedule an appointment at the UCLA Cerebrovascular Program, please call 310-825-5111 or click here to request an appointment.
