Brain vessel microsurgery is a very delicate and precise procedure that can be used to repair many vascular conditions including aneurysms, arteriovenous malformations, carotid artery stenosis, chronic venous insufficiency, and other vascular conditions. Brain vessel microsurgery is performed with the help of microscopes and long thin instruments called microsurgical instruments.
Brain vessel microsurgery procedures include:
Microsurgical clipping is a surgical procedure where metal clips are used to cut off blood flow to the aneurysm. In a craniotomy, an opening in the skull is made to reach the blood vessel. A clip is placed on the neck of the blood vessel to obstruct blood flow and stays inside the brain.
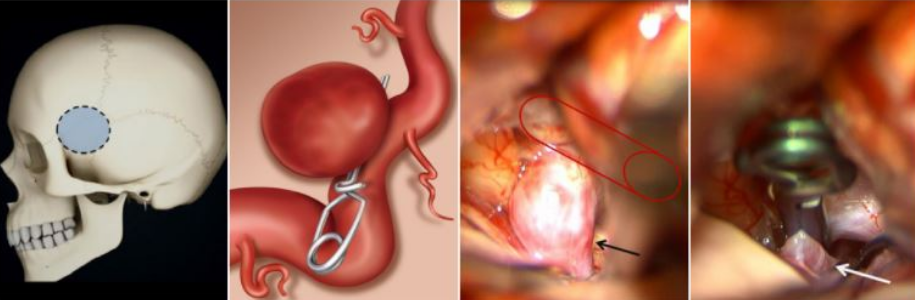
Figure 1. Microsurgical clipping. a) The outline of a typical craniotomy for aneurysm clipping. b) illustration of an aneurysm clip placed across the neck of an aneurysm, blocking blood flow into it while keeping the normal vessel open. c) Surgical images showing a right carotid artery (Red outline) aneurysm (arrow) before aneurysm clipping. d) The same surgical image immediately after clip placement on the brain aneurysm, curing it.
Artery occlusion and bypass is a two-part procedure that combines open microsurgery with endovascular coiling. This procedure provides the opportunity to coil the entire diseased portion of the blood vessel and then provide an alternative arterial supply to a specific location in the brain.
The difference between this procedure and endovascular coiling is that coiling only closes or blocks up the aneurysm sac, whereas artery occlusion and bypass the vessel is completely closed down.
Bypass is the first part of the procedure. This is an open microsurgical technique where a donor vessel from another position is attached and redirected to feed blood to a specific area of your brain that needs it. The donor vessel is detached at one point in its natural location and rerouted into a position beyond the aneurysm. It is then reattached to the parent vessel to ensure that blood continues flowing.
After the blood vessel has been bypassed, this surgery continues with a second process called occlusion where an endovascular technique called coiling is used to close (occlusion) the diseased portion of the blood vessel containing the aneurysm.
There are two methods to perform a carotid endarterectomy. General anesthesia is administered or intravenous sedation with a local anesthetic is used.
During the procedure, an incision is made in the neck at the site of the carotid artery blockage. The cerebrovascular surgeon using a microscopic camera locates and removes plaque from the artery. When complete, the surgeon closes off the wound with stitches, restoring circulation to previously blocked areas of your brain.
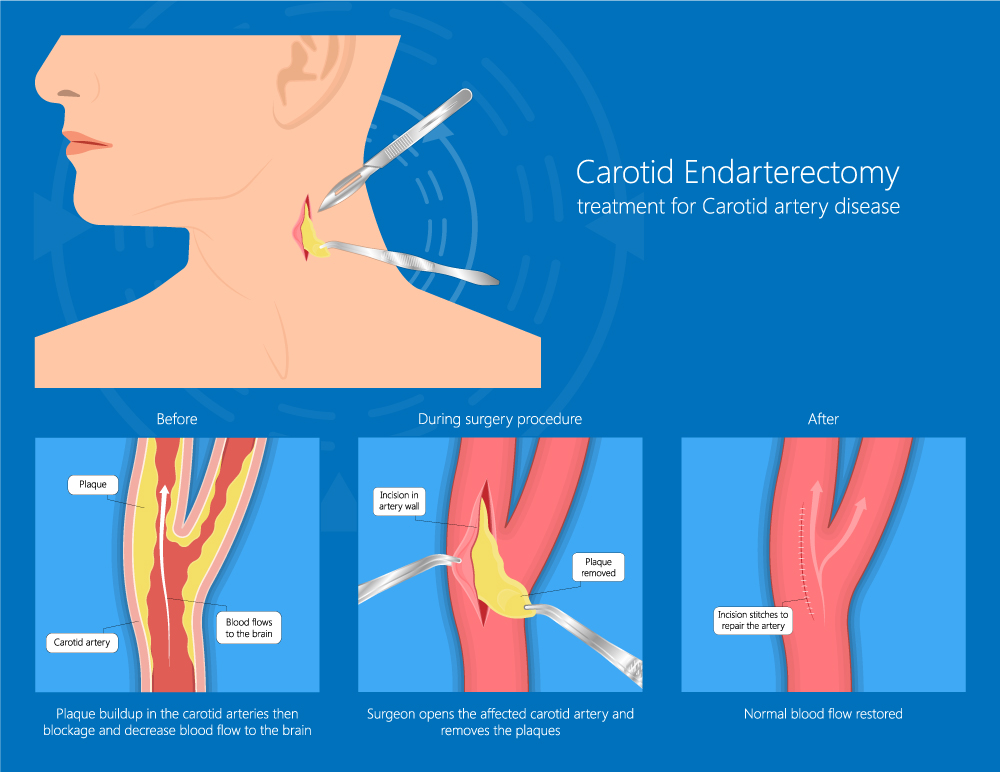
Figure 2. Carotid Endarterectomy
A direct revascularization, also known as STA-MCA bypass or EC-IC bypass, is an open surgical technique in which a blood vessel from the head (superficial temporal artery; STA) is cut and directly connected with a target vessel on the surface of the brain’s brain (middle cerebral artery or MCA).
By “bypassing” the blocked vessel at the base of the brain and creating a new blood flow pathway into the brain beyond the blockage, this operation increases blood flow to the brain right away. The sutured vessel continues to grow and deliver more blood throughout time.
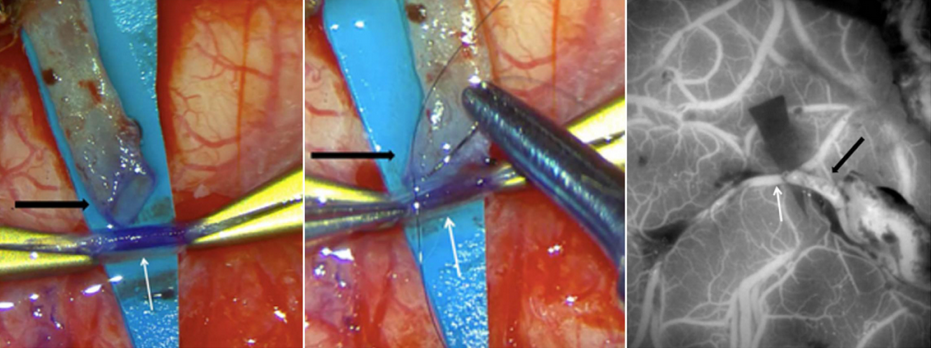
Figure 3: Images from a STA-MCA bypass surgery showing (a) the cut STA (black arrow), which has been dissected from the scalp and trimmed in preparation for use as a bypass donor, and prepared suture into the brain MCA vessel (white arrow), (b) the open end of the STA (black arrow) is being sutured onto the open MCA vessel (white arrow) and (c) intraoperative ICG dye angiogram showing blood flow through the skin vessel (black arrow) into the brain vessel (white arrow).
There are several alternatives to a “passive” bypass that will aid in the circulation of blood to a moyamoya patient’s brain. The indirect techniques all require open surgery to implant healthy extracranial tissues with adequate blood supply on the surface of the brain, after which over time develop new arteries into the brain, providing much-needed extra blood flow.
These procedures are frequently utilized in children since the tiny blood vessels are difficult to manipulate with direct bypasses. Therefore, surgeons employ a variety of techniques, such as:
Encephalo-Duro-Arterio-Synangiosis (EDAS): The superficial temporal artery (STA) from the scalp is utilized in this most common indirect bypass. Rather than cutting and suturing the STA directly to the brain blood vessels, it is left intact and draped over the surface of the brain in this technique. With time, the vessel contributes new branches to the brain, which is essential for obtaining adequate blood flow. New blood vessel formation generally takes three to six months but may continue to improve over years.
Encephalo-Myo-Synangiosis (EMS): This is a similar technique to the EDAS. But in this procedure, the temporalis muscle – which is located above the skull near the temple – is inserted through an aperture in the skull and into the brain surface. New blood flow is established from muscular vessels to brain vessels after three to six months.
Encephaloduroarteriomyosynangiosis (EDAMS): This is a hybrid procedure that combines the EDAS and EMS techniques. The brain, dura, and muscle are all positioned on top of the brain’s surface.
Multiple Burr Holes: This is a surgical procedure that can be performed on infants and children. The small brains of children tend to grow new blood vessels from tiny regions of connection with extracranial tissues via many little holes drilled in the skull.
Omental Bypass: This surgical technique is unusual and is mostly done when alternative bypass techniques have proved ineffective. This procedure consists of removing fatty tissue from the abdomen and tunneling it underneath the skin, then transplanting it on to the surface of the brain. Vascularized fatty tissue with a blood supply from abdominal arteries may also grow new vessels into the brain.
This is an open operation that requires general anesthesia and involves the resection (removal) of the cavernous malformation, which the cerebrovascular surgeon may fully remove without causing harm to surround brain tissue. Symptoms typically go away immediately following surgery.
Reserved for cases that cannot be treated with endovascular embolization. During microsurgical excision, the neurosurgeon makes a craniotomy and uses the microscope to distinguish the DAVF from the surrounding brain and spinal cord tissues. A small portion of the DAVF is removed and the remainder is sealed off to provide a cure.
The surgeon makes an incision to remove the AVM in this method, taking care to avoid injuring the spinal cord and other adjacent regions. When the AVM is tiny and located near a section of the spinal cord that is easy to access, surgery is usually done from inside the spinal canal. For larger lesions, surgery from outside the spine is typically used to remove them.
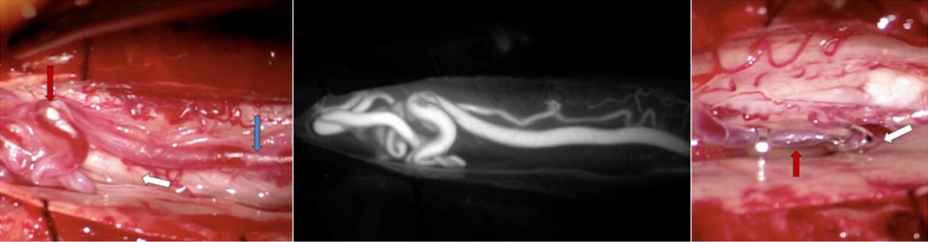
Figure 4a: Intraoperative view of a Type 1 spinal dural fistula surgery. The enlarged vein (blue arrow) laying on the spinal nerves (white arrow) is abnormally filled with red arterial blood leading to an abnormal tangle of veins (red arrow). Figure 4b: The same view of the abnormal vessels as seen with an intraoperative ICG angiogram. Figure 4c: The abnormal vein has been clipped just as it enters the spinal dura (white arrow) to stop the high arterial flow. Upstream, the vein loses its enlarged red shape and appropriately softens (red arrow) and becomes a blue-purple color like normal veins. This technique cured the fistula and the patient improved greatly.
