A brain aneurysm is a balloon-like bulge in the blood vessel wall and it is caused by a weakening of the artery’s walls that causes them to slowly stretch and grow over time. Aneurysms pose danger because as they slowly expand, they can rupture leading to blood exiting the vessel through a tear in the aneurysm and bleeding into the fluid space around the brain. An aneurysm bleed is called a subarachnoid hemorrhage and is a life-threatening medical emergency. Aneurysms, if found, can be treated before they start to bleed in order to lessen the possibility that they will bloat and rupture.
Six and a half million people in the United States have unruptured brain aneurysms (1:50) but rupture is far less common at approximately 8 out of every 100,000 people. Every brain aneurysm is different, so it’s important to have a conversation about your individual situation with brain aneurysm experts.
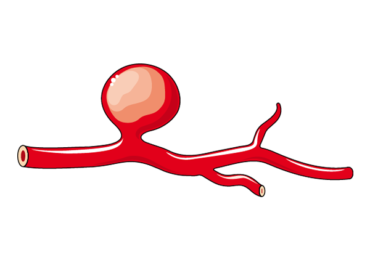
Figure 1. Saccular Aneurysm
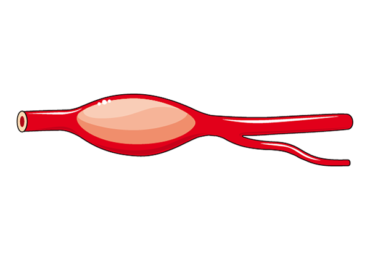
Figure 2. Fusiform Aneurysm
Though most aneurysm formation is unclear, certain factors are known to increase the risk of developing brain aneurysms such as cigarette smoking, chronic high blood pressure, chronic alcohol use, illicit drug use, and rare genetic diseases.
Brain aneurysms that have “bled” or “ruptured,” need urgent treatment. For aneurysms that have not ruptured, the risk of future rupture is largely determined by its size and location. Small aneurysms have a lower risk of rupturing and are often monitored without surgery, whereas large aneurysms are more likely to rupture and often require treatment. However, some aneurysms with specific features may need treatment at a smaller size such as aneurysms located in the vessels in the back portion of the brain, aneurysms that are monitored but noted to grow over time or develop irregular walls. Other factors may influence physicians to recommend aneurysm treatment including, patients with multiple aneurysms, individuals that have experienced a previous ruptured aneurysm, evidence of aneurysm leak and/or nerve compression; irregular aneurysm wall outpouching and history of aneurysms in multiple family members. When to treat vs monitor a brain aneurysm is an important decision and should be made in conjunction with a brain aneurysm specialist.
Brain aneurysms are most commonly discovered when brain imaging is performed for other reasons and the aneurysm is “incidentally” discovered. These asymptomatic aneurysms are managed differently than aneurysms that have leaked blood where brain bleeding is present.
Symptoms of aneurysm rupture and bleeding around the brain typically include, severe and sudden headaches often described as “the worst headache of my life”; followed by nausea and vomiting, drowsiness or confusion.
If you or someone you know has experienced these symptoms contact a doctor immediately because it is a time sensitive condition that needs treatment urgently!
An aneurysm can be diagnosed through brain blood vessel imaging studies:
Magnetic Resonance Imaging Angiogram (MRA): Uses a magnetic field to create and display images of blood vessels in the brain.
Computed Tomography Angiogram (CTA): Using multiple X-ray images taken from different angles the CTA allows the doctor to see cross-sectional pictures of the brain and blood vessels. Contrast dye makes vessels more visible, it is often injected into an arm vein via an IV in order to get a better look at blood vessels.
Cerebral Angiogram (Digital Subtraction Angiography): Cerebral angiograms are the most accurate way to diagnose brain aneurysms. During a cerebral angiogram, small tubes are introduced into the arm or leg artery, advanced inside the blood vessels under x-ray guidance to the neck vessels leading to the brain. Contrast dye is injected through the tubes into the neck blood vessels where it travels with blood flow towards the head and fills the brain vessels while images are obtained demonstrating the blood vessels in excellent detail.
Ruptured brain aneurysms require treatment before the patient leaves the hospital. Unruptured brain aneurysms can either be treated or observed. The decision to treat or observe an unruptured aneurysm is nuanced based on numerous patient and aneurysm related factors. Your cerebrovascular neurosurgeon will help guide you through the different options for treatment and best way to proceed based on your individual case. In general, there are different techniques to treat brain aneurysms, such as surgical clipping and endovascular treatments (neurointerventional treatments) including:
- Endovascular coiling
- Endovascular stent-assisted coiling
- Endovascular flow diversion
- Endovascular Intrasaccular flow diversion (WEB device)
Open Surgical Treatments
- Surgical Aneurysm Clipping
- Aneurysm Trapping and Bypass
A variety of surgical and endovascular treatment tools are available for treating brain aneurysms, and which type of treatment plan is best for a given patient is very much tailored to the individual patient and should be discussed with an expert cerebrovascular neurosurgeon.
Endovascular surgery is a minimally invasive treatment that has been used to treat many different neurovascular conditions such as aneurysms, vascular malformations, and other arterial conditions. It involves inserting a catheter into the artery and then using it to perform an angioplasty or stent placement. Endovascular Surgery offers many benefits over traditional forms of surgery such as faster healing times and smaller incisions.
Since its conception, endovascular treatment has rapidly taken over as the major treatment for most intracranial aneurysms including:
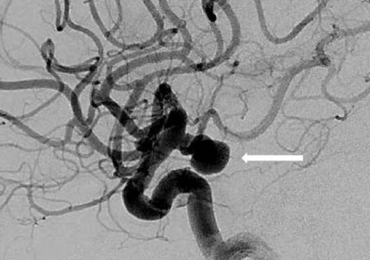
Endovascular coiling is the process by which an aneurysm is blocked with coils to stop blood flow. This is a minimally invasive procedure, meaning that instead of cutting into the skull to treat aneurysms in the brain, it’s done by inserting catheters up through arteries until it reaches the damaged area where platinum coils are released to coagulate (embolization) the aneurysm and prevent blood from entering it.
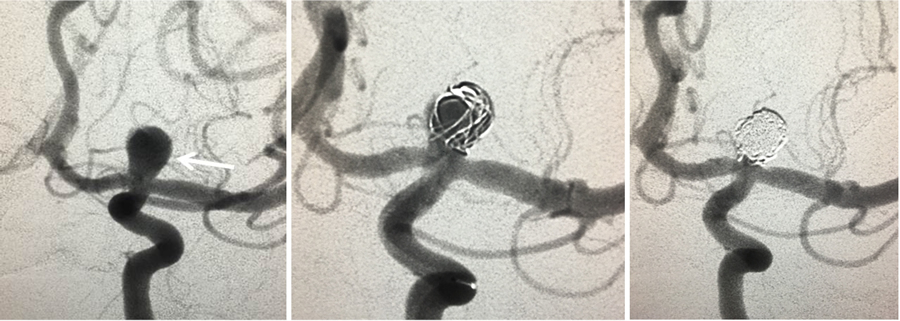
Figure 3. Anterior 2D angiographic view of a cerebral aneurysm (white arrow) located at the left carotid artery bifurcation (left). The cerebral aneurysm after one coil has been placed inside the aneurysm (middle) and the final image (right) after the coiling has been completed demonstrating aneurysm occlusion.
Stent-assisted coiling is when coils are inserted alongside a stent to compress the aneurysm and seal it off from blood flow. The stent is placed across the base of the aneurysm to act as a scaffold to keep the coils in place.
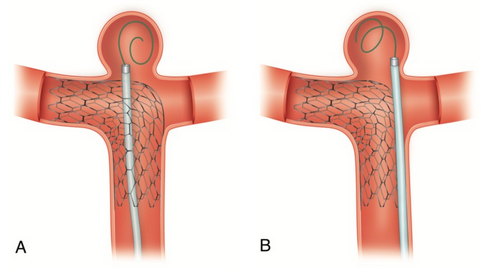
Figure 4. Stent-assisted coiling. (A) Coil-through struts technique. B) Jailing technique.
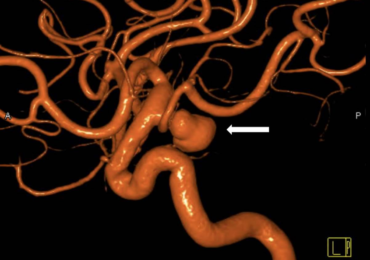
In the flow diversion procedure, a metal stent made with fine holes is precisely placed inside the brain vessel covering the aneurysm base or neck. The stent diverts blood flow away from the aneurysm while allowing normal flow to the brain. Over several months, the aneurysm shrinks and often completely resolves and the brain artery remains open. This technique is often used for very large or difficult-to-treat aneurysms.
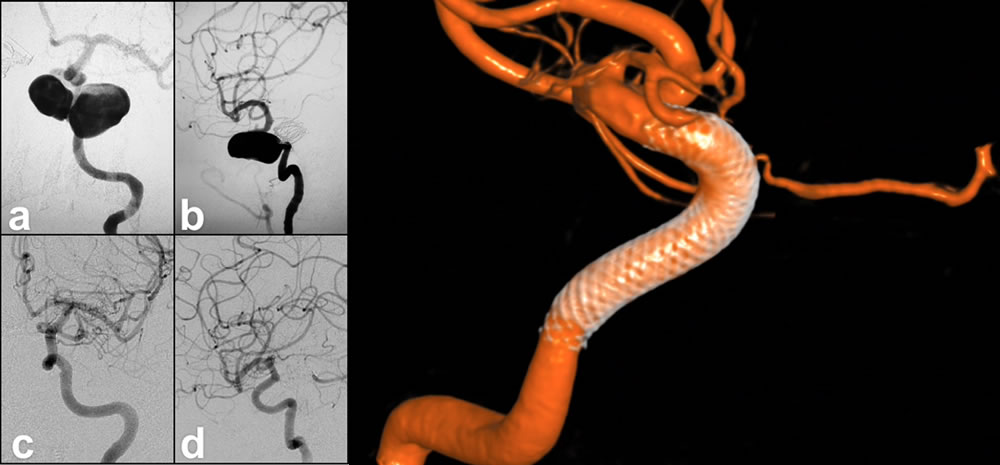
Figure 5. Giant, tri-lobed left ICA cavernous segment aneurysm pre-treatment (a) AP and (b) lateral angiographic views. Six months post-treatment with pipeline flow diverting stent shows complete obliteration of the aneurysm on (c) AP and (d) lateral views. (e) shows the pipeline stent in the vessel after the aneurysm has occluded.
Microsurgical clipping is a surgical procedure where metal clips are used to cut off blood flow to the aneurysm. In a craniotomy, an opening in the skull is made to reach the blood vessel. A clip is placed on the neck of the blood vessel to obstruct blood flow and stays inside the brain.
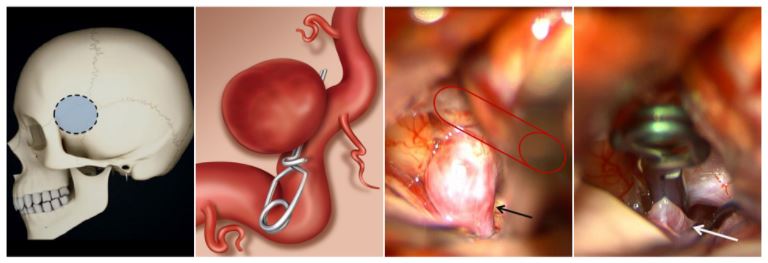
Figure 6. Microsurgical clipping. a) The outline of a typical craniotomy for aneurysm clipping. b) illustration of an aneurysm clip placed across the neck of an aneurysm, blocking blood flow into it while keeping the normal vessel open. c) Surgical images showing a right carotid artery (Red outline) aneurysm (arrow) before aneurysm clipping. d) The same surgical image immediately after clip placement on the brain aneurysm, curing it.
Artery occlusion and bypass is a two-part procedure that combines closure (trap) of a diseased portion of the vessel and bypass which creates blood flow beyond the occlusion point.
Bypass is an open microsurgical technique where a donor vessel is detached at one point in its natural location and rerouted into a position beyond the aneurysm. It is then reattached to the parent vessel to ensure that blood continues flowing.
After the blood flow rerouting strategy has been made (bypass)the diseased portion of the blood vessel containing the aneurysm can be occluded with either trapping with clips or endovascular coils.
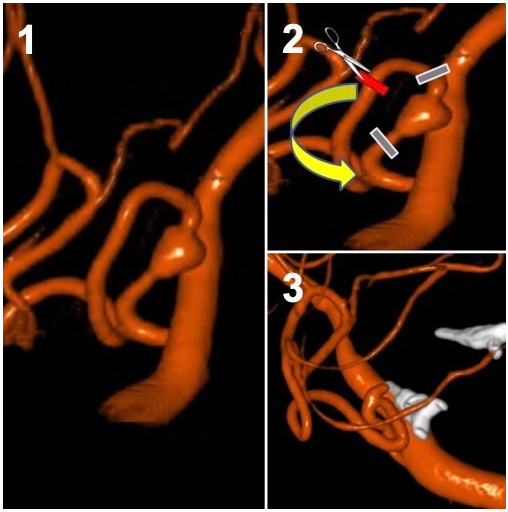
Figure 7. Trap and bypass of a ruptured dissecting Posterior Inferior Cerebellar Artery (PICA) aneurysm. 1. Lateral view of the dissecting aneurysm (arrow). 2. Demonstration of the planned clip locations (grey bars) to trap the aneurysm and the cut (red bar) with the proposed reconnection (bypass) to reconnect the artery to the blood flow and prevent a stroke. 3. After the trapping (white clips) and bypass there is preserved blood vessel flow and the aneurysm is trapped between the clips and is no longer at risk of rupture.
Brain aneurysm management is complex and should be tailored to the individual aneurysm and the individual circumstances of each patient. When to treat vs monitor a brain aneurysm is an important decision and should be made in conjunction with a brain aneurysm specialist.
